If you and your partner have been trying to conceive for over a year without success, or if a woman over 35 has been trying for more than 6 months with no results, it may be time to consider infertility testing. Professional testing can help identify potential causes and allow for timely treatment.
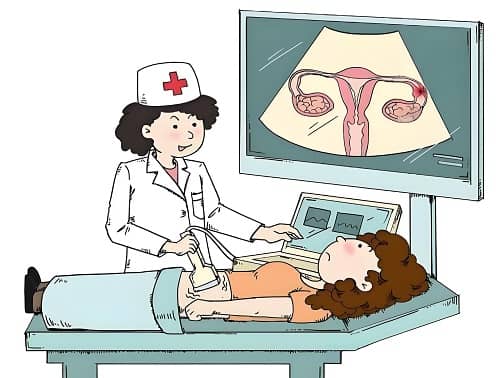
Table of Contents
- Female Infertility Testing
- Male Infertility Testing
- Considerations When Undergoing Infertility Testing
Female Infertility Testing
- Ovulation Function Testing
This includes monitoring basal body temperature, ultrasound follicle monitoring, and hormone level testing (such as FSH, LH, and estradiol) to assess whether ovulation is occurring properly. - Fallopian Tube Patency Testing
- Hysterosalpingography (HSG): This X-ray procedure helps determine whether the fallopian tubes are open or blocked. A blocked tube can prevent the sperm from reaching the egg, leading to infertility.
- Uterine Testing
- Ultrasound: Used to check the shape of the uterus and identify any abnormalities such as fibroids or uterine malformations that could affect fertility.
- Hysteroscopy: A procedure that allows for direct observation of the uterine lining to check for polyps, adhesions, or other issues that could interfere with implantation.
- Endocrine Testing
Blood tests are used to check hormone levels such as thyroid hormones, prolactin, and insulin, which can influence fertility. Hormonal imbalances may interfere with ovulation and overall reproductive health. - Pelvic Testing
Pelvic exams help identify conditions like pelvic inflammatory disease (PID) or endometriosis, which can interfere with fertility by affecting the reproductive organs.
Male Infertility Testing
- Semen Analysis
Semen analysis tests for sperm count, motility, morphology, and overall semen quality. This is a fundamental test for assessing male fertility and helps identify potential issues such as low sperm count or poor sperm motility. - Genital Examination
Ultrasound or physical exams are used to assess the development of the testes and detect conditions like varicocele or orchitis, which can affect sperm production and quality. - Hormone Level Testing
Testing for gonadotropins (FSH, LH) and testosterone levels helps evaluate male endocrine function, as these hormones regulate sperm production. - Chromosomal and Genetic Testing
For men with severe oligospermia (low sperm count), azoospermia (no sperm), or recurrent miscarriages, genetic testing can identify conditions like Klinefelter syndrome or other hereditary issues that might affect fertility.
Considerations When Undergoing Infertility Testing
- Choose a Reputable Clinic
It’s important to select a fertility clinic or hospital with the appropriate reproductive medicine credentials to ensure accurate and professional testing results. - Both Partners Should Be Tested
Infertility can be caused by factors from either or both partners, so it’s essential that both partners undergo testing to identify the root cause of the problem. - Maintain a Positive Outlook
The process of infertility testing and treatment can be emotionally taxing, but it’s important to stay positive. Testing is just the first step toward resolving the issue, and most patients can improve their fertility with appropriate treatment.
Infertility testing is a key step in identifying the causes of infertility. Early diagnosis and treatment can significantly increase the chances of conception and help you achieve your family-building goals.